“We’ve got to educate ourselves, educate our families, educate our community, and sometimes you need to educate your doctor.”
The death of Chadwick Boseman has left a lasting impact on the African American community.
It’s an unfortunate reminder that colon cancer, like so many other diseases, disproportionately affects African Americans. Even if you’re Black Panther.
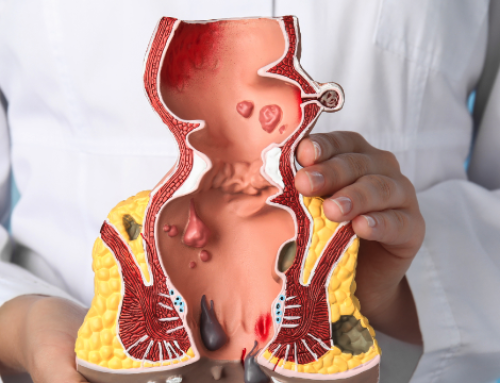
Many people are still unfamiliar with the specifics of this disease: What causes it? Who is at risk? What signs should I be looking for? How can I stave off colon cancer?
I returned to Sway’s Universe on Sirius XM and spoke with Kelly Kinkaid about the warning signs of colon cancer, how to live a healthier lifestyle and more.
Listen to our conversation below.
Transcription
Kelly Kinkaid: Welcome to First Aid with Kelly Kinkaid. Today, we have a special edition because it is timely. At First Aid, we talk about various health conditions, but this one is hitting home for a lot of us.
Recently we had news that Hollywood lost an angel. Someone who was spreading the good word, someone who was a superhero to many. Chadwick Boseman passed away at the age of 43 from colon cancer. Today I wanted to bring in a guest who is a friend to the show, Dr. Lynn O’Connor, to talk about this. Dr. O’Connor is a colorectal physician and is at work and took the time out to talk to us about this disease. Dr. O’Connor, how are you doing today?
Dr. Lynn O’Connor: Thank you so much for having me, Kelly. This is such an important topic and I’m glad we’re discussing but under, unfortunately, unfortunate circumstances. But I’m glad we are discussing it.
Kelly Kinkaid: When we talk about colon cancer, colon cancer is one of the top 3 cancers that causes death now?
Dr. Lynn O’Connor: It’s actually the third most common cancer in the United States. And it is the second most cause of cancer death. In 2020, we expect to have anywhere from 140,000 cases and over 50,000 deaths from colon cancer. The problem is, 11% of the cases of colon cancer are in those under 50.
Kelly Kinkaid: That’s what I find so alarming now because when you think about colon cancer and the colon, going to the doctor to get your annual exam, when you get to the age of 50 you know you have to go get your colonoscopy. But that is changing now because we’re told to get our colonoscopy earlier now. What’s the age? When should people be getting colonoscopies now?
Dr. Lynn O’Connor: Initially, colon cancer was traditionally a cancer that was looked at in older folks. 68 to 72 years of age was the average age we were seeing colon cancer. It occurs in all races, all ethnicities, men and women, but we have found it more disproportionately in African Americans. When you’re looking to get a colonoscopy, the traditional age was 50. Because of the increase in incidents in younger patients, we’ve seen about a 50% increase in younger patients since 1994, the American Cancer Society decreased the age from 50 to 45. Now we’re asking average-risk individuals – average-risk meaning people who don’t have any history of colon cancer, don’t have any history with colon polyps, they don’t have any medical predispositions or they don’t have IBS or other signs and symptoms – to get a colon screening at age 45.
Kelly Kinkaid: I want to ask, what are some symptoms or some signs…but also, the age is getting younger now. And the demographics – African Americans are being diagnosed with colon cancer. Why do you think that’s so?
Dr. Lynn O’Connor: It’s unfortunate. Across all cancer, African American men and women and more predisposed to decreased survival and higher mortality and our cases are there. I think it’s significantly because access to care, disparities in care, access to screening. Some of the risk factors are obesity, sedentary lifestyle, we’re not getting up, we’re not moving. Especially now, most of the gyms are closed. Our diet – diets high in fat, fatty foods, high in nitrates, processed foods like cold cuts and bacon.
We’re just not doing what we need to do. We’re not exercising. The American Heart Association recommends at least 30 minutes of exercise at moderate intensity 5 days a week and that can help stave off colon cancer. But it’s those risk factors that really are a problem. And one of the main problems, as I said earlier, is access to healthcare. Disparities in healthcare and disparities in screening in the African American community really contribute to what we are seeing.
Kelly Kinkaid: Dr. Lynn, let’s be real. We’re talking about colon cancer because of Chadwick Boseman, right? He was 43 years old. He was Black Panther, he was fit, he looked good. Then during the end of his when we didn’t know he was doing chemotherapy he had a weight loss that you could really see, it was a drastic weight loss. But you’re thinking…I keep on saying, “He was Black Panther!” He was in all these movies looking fit and all. But what I’ve read is that he didn’t discover that he had colon cancer until Stage III. So what should we be looking for in addition to getting to a certain age. What are the signs and symptoms?
Dr. Lynn O’Connor: It’s unfortunate too because he died at age 43 but 4 years earlier he was age 39. The problem is when you do have these younger patients and we do have these signs and symptoms like weight loss, blood in our stool, change in our bowel habits – whether you have pencil thin stool, you’re not going as much, you’re constipated, you have diarrhea – something that’s not your normal.
Those are the signs and symptoms we look at but those are the symptoms that are advanced. By the time we see those signs and symptoms, our disease is advanced. The problem with African Americans and younger patients when they present is they present with advanced disease. And the reason being is 73% present with advanced. 82% of younger patients, we’re talking younger on-set who are 50 years or younger, are misdiagnosed because nobody is thinking about these symptoms. Nobody is thinking that a 39 year old with some rectal bleeding has colon cancer. It’s not registering, “Let’s do a colonoscopy”.
Another thing is, we’re not talking about it with our families. We don’t know our family history, we don’t know what our grandma and grandpa had, we don’t know what our cousins, aunts and uncles had. We don’t know if there’s cancer in the family. So we’re not educating ourselves and a lot of our physicians are not educated to look for these issues and discuss it with younger patients.
Kelly Kinkaid: When you talk about stool, I think for me, I do always advocate. I am my first doctor and you have to know your body. But how do you determine…say you had a bad pick of a Mexican restaurant or a bad burrito and you have diarrhea for a couple of days because that bug just didn’t get out. Sometimes I think with the state of COVID and all of these people dying of different things we’re becoming hypochondriacs. I guess my question is if there’s a little blood in your stool and you’re constipated because maybe you didn’t have enough water this week, when should you be alarmed?
Dr. Lynn O’Connor: First, it’s completely understandable with the state that we’re in with COVID and there’s so many symptoms associated with COVID that we’re finding. But what you want to look for is a sustained change in your bowel habits. Obviously we all have that Montezuma’s Revenge and have Mexican food or White Castle and it will run right through you. And that’s understandable. But if you notice that you’re eating healthy and you’re still having diarrhea and it’s a sustained change for 2-3 weeks, this is something that’s different.
Not everybody moves their bowels everyday but if you’re noticing it’s going every 4 days or every 5 days, that’s when you know something’s changed. If you’re losing weight and you’re not trying to something’s changed. Blood in the stool is not normal no matter what. The majority of the time when patients come to me, 84% of the time it’s from hemorrhoids, a fissure or abscess. But you can’t just say that. You have to get it checked. Even if there is something wrong it doesn’t have to necessarily be colon cancer, but get it checked. That’s the thing that’s important. Get a screening if you have to.
When you’re talking about these signs and these symptoms, we’re talking about sustained change. Not just a day, not just a week, not just a binge of improper food, or not drinking enough water or eating beets. Sometimes eating foods like foods or certain medications like aspirin can cause a change in your stool. It can make it look like it’s red. Even certain medications. You just have to check with your doctor if there’s any questions. These are things to make you think. These are things to make you realize this is not normal. This may be a sign, this may be a symptom. Let me get checked.
Kelly Kinkaid: I think with everything going on, with many people passing away and that younger rate, it becomes so alarming to see. But looking on the bright side, I want you to speak on how important early detection is. Because you can survive…there’s a survival rate for colon cancer.
Dr. Lynn O’Connor: There are a ton of survival rates for colon cancer which is why we’re advocating early screening which is why we’re advocating getting screening. Why we’re advocating getting checked.
Kelly Kinkaid: What I’d like to speak about more is that early detection is key. Speak about early detection. We’ve already said, at the age of 45, if you see blood in your stool go to the doctor. But if you’re at Stage I or II what are some things you would advise or advocate for someone when they get that diagnosis?
Dr. Lynn O’Connor: Well we talked about early detection being key. Having a colonoscopy and having a polyp removed before it turns into a cancer. And if you do find a cancer and it’s in early stage, they should have a 95% 5-year survival if it’s removed early. For those patients who have had symptoms, they went to their doctor, they had a colonoscopy and now they are positive and they have the diagnosis of colon cancer. The most important thing is to one, keep your spirits up mentally. Get a support group because this is something that’s going to be significant to go through. And try to fortify your body, mind and soul.
Eating right – that’s still very important because you need that energy to be able to fight. Healthy foods with zinc in there and are immune boosting. You want to have fruits, you want to have vegetables, drink lots of water and rest. Rest is key because you want to prepare your body for surgery. The majority of colon and rectal cancers that are caught early are surgically removed. It’s only when you get advanced disease you are treated with chemotherapy and even if you do need chemotherapy, all that advice applies. Getting the proper rest, getting the proper food, getting the proper nutrition and having that support group around you so you can pass the treatment and pass the diagnosis and onto the cure.
Kelly Kinkaid: You spoke this word when we were talking: hemorrhoids. Is there any link between hemorrhoids and colon cancer?
Dr. Lynn O’Connor: No there is not. Hemorrhoids are pains in the bottom that come on from prolonged sitting, a lot of women who are pregnant and give birth often get hemorrhoids. Even men get hemorrhoids. But there is no link between hemorrhoids and colon cancer. Like I said, they can occur in pregnant women, sitting, standing but there is no link between that and colon cancer and rectal cancer. They are two separate entities.
Kelly Kinkaid: Once upon a time, colon cancer was usually linked toward men. But women can get colon cancer too. Like breast cancer was always pushed over to women and colon cancer was men. Speak on how the rates with women and colon cancer are rising and why is that?
Dr. Lynn O’Connor: Well colon cancer is an equal opportunity cancer. It occurs in all races, all ethnicities and both genders. But for some reason, there is a greater disposition in men than there is in women. When you look at the races, African Americans present higher stages than their Caucasian counterparts. The mortality rate is higher than their Caucasian counterparts and their survival rates are lower.
When you break it out to just African Americans, men for some reason they’re in a higher category than women. It really does happen to both men and women but men are slightly higher. And it could be simply because women are the caretakers, the nurturers of the family. We go to the gynecologist, we take our kids. So we do a little bit more of the health maintenance than men do. There was a study that I read where men, regardless if they were married or unhappily married, the married men actually live longer because their wives will take them to the doctor. It’s not the same for women, but for men their significant others will take them to the doctor.
Kelly Kinkaid: Females rule the world. Before I close out, one of my missions is to get information out. I think it’s very important. I read that by the time 2030 comes the rates of colon cancer, they’re on the rise now, but they’re going to get even worse. What can we do and what can we tell that person who doesn’t go to the doctor, who eats cold cuts and just eats bad. How can we change this narrative for all ages?
Dr. Lynn O’Connor: One of the things that’s really important is your overall health because a lot of the problems that we have stem from our lifestyle. Smoking. Clearly we know that’s linked to lung cancer, colon cancer and other cancers. Alcohol in moderation. Weight loss, obesity. We’ve got diabetes, heart attacks and stroke and kidney disease and that plagues the African American community.
So one of the things that’s important is educating younger kids early on and the parents and family is eating right. Exercising. There’s no stigma to getting out there and exercising and eating right. Leave all the McDonald’s and Taco Bell and that stuff alone. Every now and then it’s fine but it’s moderation. And those are things we need to do in the beginning. Set a foundation for a healthy lifestyle and healthy eating.
We also need to be talking to our families. That we know our family history. We need to know who had what when they had it, why they had it, where they had it. That’s important. And the third thing is making sure we’re breaking these barriers of access to care and barriers because of disparity. We’ve got to educate ourselves, educate our families, educate our community, and sometimes you need to educate your doctor. If your doctor is not going to listen to you, find another one. If someone is not going to pay attention to your signs, your symptoms, and you demand a colonoscopy and they say, “No you’re too young” you find another doctor.
Kelly Kinkaid: Are there any foods that we can take so we can have a better colon? What’s a good colon and what’s a bad colon?
Dr. Lynn O’Connor: I’ll tell you, a bad colon consists of all that takeout. The high fatty foods, the cold cuts, the processed meats. All that stuff that’s fun. Moderation is key. Labor Day is coming up. You’re going to a barbecue, have a little bit of something, fine. But if you’re having that every single day. If your diet consists of McDonald’s for breakfast, Burger King for dinner and Taco Bell for lunch, that’s not what you need.
The foods you need are the ones that are going to nourish your body and your mind. We’re talking about high fiber fruits and vegetables. Nuts, spinach, leafy greens, kale, broccoli. Fruits, grains, lots of water. And everything else in moderation. If you’re a woman you really should only have one drink a day. A man should only have two glasses of wine a day, if you are going to drink. And absolutely no smoking.
The foods you want should be healthy. You’re going to want 20 to 35 grams of fiber a day. Slowly but surely build up to it, but that’s what you’re looking for. That’s enough fiber in the diet to move that stool through.
Kelly Kinkaid: When you say fiber, for people who might not know right off the bat, what does that mean? What type of fiber?
Dr. Lynn O’Connor: For instance, if you’re going to have a bagel. Instead of getting a poppy seed white bagel, substitute for a whole wheat bagel. If you’re going to have a turkey sandwich, get the bread that’s whole grain. Multi-grain and whole grain, that’s what you’re going to look for. If you have a salad, instead of romaine or iceberg, put in some arugula, put in some kale and put in some spinach. The darker your greens are the better.
A quick way to understand if you’re eating properly is eat the rainbow. Your whole plate should not look one color. For instance, when you go to KFC, you get the pale brown biscuit, the mashed potatoes that are pale white and the chicken that’s brown. The whole plate is the same color. You need some color. You need some sweet potatoes without the sugar. You need some spinach on there, you need some kale. Even with protein, you can do fish, salmon, eggs. You can see the colors on the plate and that’s what you’re looking for.
Kelly Kinkaid: That’s simple. I think we overthink it because things taste good but there are so many things in the rainbow that taste good. It’s just hard sometimes because we’re already living in COVID.
Dr. Lyn O’Connor: And you can still eat good food! You just don’t have to fry it. You can boil it, you can steam it and add spices. There are little ways to do that. For moms who are cooking for kids, you can stick spinach in something and they’ll never know. Make a smoothie and put some spinach in. Make an egg and put some spinach in. A little tomato, some onion. Stick those things in there and you’ll be able to slowly but surely change the diet. You want to eat some Cheerios? Eat Cheerios but then throw some Fiber One on there. That way you can eat a lot of good food with a little bit of fun food. That way it doesn’t feel like you’re eating cardboard and rabbit food everyday.
Kelly Kinkaid: I want to thank you Dr. O’Connor for taking time out and for continuing to educate us. Last time you were here is was so educational, it was fun and engaging. I want people to live, that’s why I do this and I know you put in the hours to educate people so they can live healthier lifestyles so thank you.